High-Risk Pregnancy And Fetal Development: Addressing Growth Restriction
High-risk pregnancies pose significant challenges for both expectant mothers and healthcare providers, requiring specialized monitoring and intervention to ensure the health and well-being of both mother and baby. One of the complications that can arise in high-risk pregnancies is fetal growth restriction (FGR), also known as intrauterine growth restriction (IUGR). FGR occurs when a fetus fails to reach its expected growth potential in the womb, potentially leading to serious health consequences. In this article, we delve into the causes, consequences, and management of fetal growth restriction in high-risk pregnancies.
To Know More About It Please Click Here
Understanding Fetal Growth Restriction
Fetal growth restriction occurs when a fetus fails to reach its expected growth potential based on gestational age. This can manifest as a decrease in the size of the fetus, particularly in measurements such as abdominal circumference, head circumference, and estimated fetal weight. FGR can be classified as either symmetric or asymmetric:
Symmetric FGR: In symmetric FGR, all parts of the fetus are proportionally small, indicating that growth restriction occurred early in pregnancy and affected the overall development of the fetus.
Asymmetric FGR: Asymmetric FGR occurs when the fetus has a normal-sized head but smaller abdominal circumference, suggesting that growth restriction occurred later in pregnancy and primarily affected the growth of the abdomen.
Causes and Risk Factors
Fetal growth restriction can be caused by a variety of factors, including maternal, placental, and fetal factors:
Maternal Factors: Maternal conditions such as hypertension, diabetes, chronic kidney disease, autoimmune disorders, and malnutrition can impair placental function and restrict fetal growth.
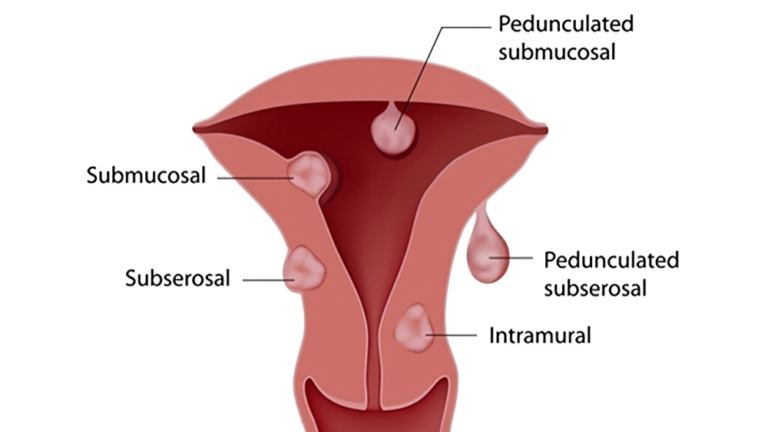
Placental Factors: Placental insufficiency, characterized by inadequate blood flow and nutrient delivery to the fetus, is a common cause of fetal growth restriction. Placental abnormalities, such as placental abruption, placenta previa, and placental infarctions, can also contribute to FGR.
Fetal Factors: Genetic abnormalities, chromosomal disorders, congenital infections, and multiple gestations (twins, triplets) can increase the risk of fetal growth restriction.
Other risk factors for FGR include maternal age (teenage mothers and women over 35), smoking, drug use, alcohol consumption, and socioeconomic factors such as poverty and inadequate prenatal care.
Consequences of Fetal Growth Restriction
Fetal growth restriction can have serious consequences for both the fetus and the newborn:
Increased Risk of Stillbirth: FGR is associated with an increased risk of stillbirth, particularly if severe growth restriction is present.
Neonatal Complications: Infants born with FGR are at increased risk of preterm birth, low birth weight, small for gestational age (SGA), hypoglycemia, hypothermia, respiratory distress syndrome (RDS), and neonatal intensive care unit (NICU) admission.
Long-Term Health Effects: FGR has been linked to an increased risk of developmental delays, cognitive impairment, metabolic syndrome, cardiovascular disease, and other chronic health conditions later in life.
Diagnosis and Monitoring
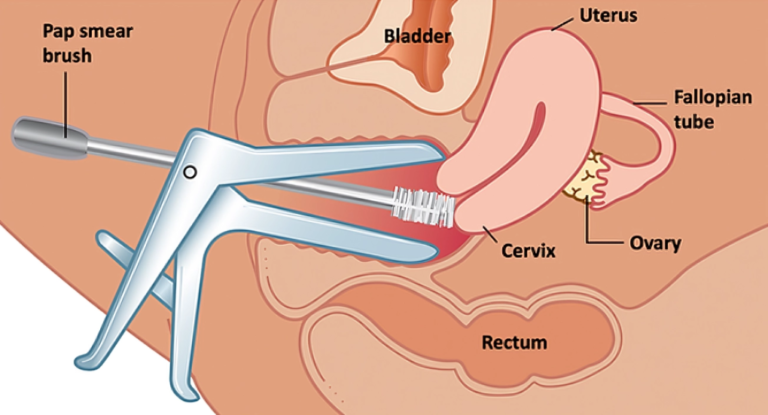
Diagnosing fetal growth restriction typically involves a combination of clinical assessment, ultrasound evaluation, and fetal monitoring:
Ultrasound: Serial ultrasound measurements of fetal biometry, including abdominal circumference, head circumference, and femur length, are used to estimate fetal growth and monitor for signs of growth restriction.
Doppler Ultrasound: Doppler ultrasound can assess blood flow in the umbilical artery, uterine artery, and fetal middle cerebral artery, providing valuable information about placental function and fetal well-being.
Fetal Monitoring: Non-stress tests (NSTs), biophysical profiles (BPPs), and contraction stress tests (CSTs) may be used to assess fetal heart rate variability, fetal movements, and amniotic fluid volume, helping to evaluate fetal well-being.
Management and Treatment
Management of fetal growth restriction in high-risk pregnancies focuses on monitoring fetal well-being, optimizing maternal health, and timing delivery to minimize complications:
Fetal Surveillance: Close monitoring of fetal growth, umbilical artery Doppler studies, and fetal well-being assessments are essential for identifying signs of deterioration and determining the need for intervention.
Maternal Management: Management of underlying maternal conditions such as hypertension, diabetes, and autoimmune disorders is critical for optimizing placental function and fetal growth.
Timing of Delivery: In cases of severe fetal growth restriction or evidence of fetal compromise, early delivery may be necessary to prevent adverse outcomes. The timing of delivery is individualized based on gestational age, fetal size, placental function, and maternal health status.
To Know More About It Please Click Here
Conclusion
Fetal growth restriction is a serious complication of high-risk pregnancies, requiring close monitoring and intervention to optimize maternal and fetal outcomes. By understanding the causes, consequences, and management strategies for FGR, healthcare providers can provide comprehensive care for expectant mothers and their babies. Early detection, timely intervention, and multidisciplinary collaboration are essential for minimizing the risks associated with fetal growth restriction and ensuring the best possible outcome for both mother and baby. Through targeted interventions and ongoing support, we can improve the prognosis for infants affected by FGR and promote healthy development and well-being from pregnancy through infancy and beyond.