Understanding and Managing Urine Infection for Optimal Health
Urine infections, though common, can significantly impact one’s daily life and overall well-being. In this comprehensive blog post, we will delve into the intricacies of urine infections, exploring their causes, symptoms, and most importantly, effective strategies for managing and preventing them. By understanding the nuances of urine infections, you can take proactive steps to safeguard your health and promote optimal well-being.
What is a Urine Infection
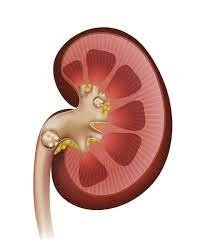
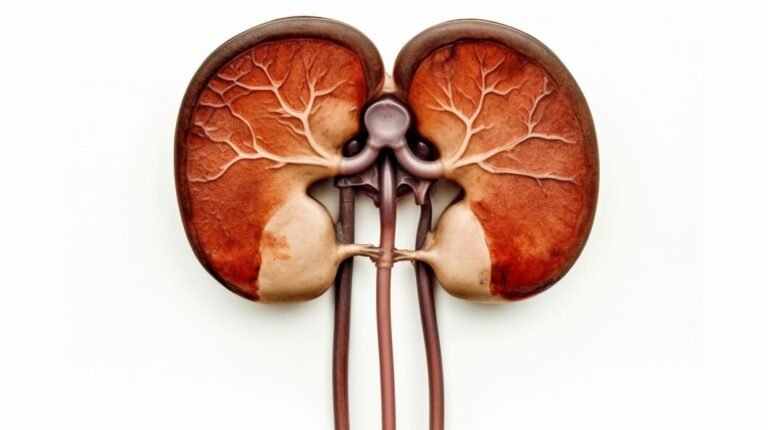
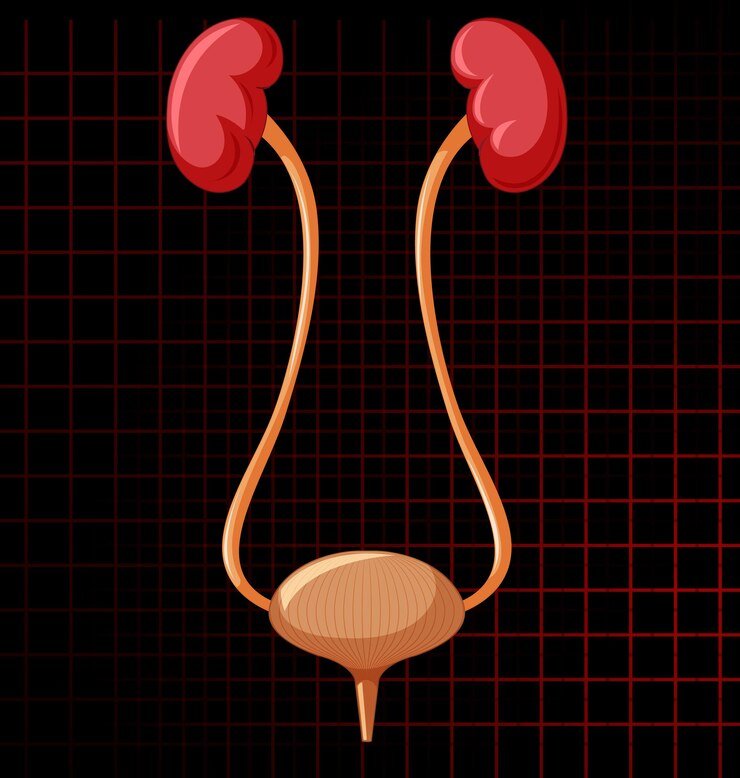
A urine infection, also known as a urinary tract infection (UTI), occurs when bacteria enter the urinary tract, leading to an infection. The urinary tract comprises the kidneys, bladder, ureters, and urethra. UTIs can affect any part of this system, with lower urinary tract infections (involving the bladder and urethra) being more common than upper urinary tract infections (involving the kidneys).
Causes and Risk Factors
Understanding the causes and risk factors of urine infections is crucial for effective management. Common causes include the presence of bacteria, usually Escherichia coli (E. coli), in the urinary tract. Risk factors include gender (women are more prone to UTIs), age, sexual activity, urinary tract abnormalities, and weakened immune systems. Recognizing these factors can help individuals take preemptive measures to reduce their risk of developing a UTI.
Signs and Symptoms
Identifying the signs and symptoms of a urine infection is essential for prompt diagnosis and treatment. Common symptoms include a frequent urge to urinate, a burning sensation during urination, cloudy or strong-smelling urine, and pelvic pain. Understanding these indicators allows individuals to seek medical attention early, preventing the infection from worsening.
Diagnosis and Medical Intervention
Proper diagnosis is crucial for determining the most effective course of treatment. Medical professionals typically use urine tests to detect the presence of bacteria and assess the severity of the infection. Depending on the diagnosis, antibiotics may be prescribed to eliminate the bacteria causing the infection. It is vital to complete the full course of antibiotics as prescribed by a healthcare provider to ensure complete eradication of the infection.
Prevention Strategies
Preventing urine infections involves adopting proactive lifestyle changes and hygiene practices. Staying hydrated, practicing good genital hygiene, avoiding irritating feminine products, and urinating promptly after sexual activity are essential preventive measures. Additionally, wearing breathable cotton underwear and avoiding tight-fitting pants can help maintain a healthy urinary tract.
Natural Remedies and Lifestyle Adjustments
In addition to conventional medical treatments, incorporating natural remedies and lifestyle adjustments can complement the management of urine infections. Drinking unsweetened cranberry juice, taking probiotics, and maintaining a balanced diet rich in antioxidants can support overall urinary health. Stress management techniques, such as yoga and meditation, may also play a role in preventing recurrent infections.
Seeking Timely Medical Attention
Recognizing the importance of seeking prompt medical attention is crucial for managing urine infections effectively. Delayed treatment can lead to complications and recurrent infections. Individuals experiencing persistent or worsening symptoms should consult a healthcare professional for a thorough evaluation and personalized treatment plan.
The Role of Hydration in Urinary Health
Hydration plays a pivotal role in maintaining urinary health. Consuming an adequate amount of water helps flush out bacteria from the urinary tract, reducing the risk of infection. Understanding the connection between hydration and urinary health empowers individuals to make conscious choices that positively impact their overall well-being.
Addressing Recurrent Infections
For individuals prone to recurrent urine infections, a proactive approach is essential. This may involve working closely with a healthcare provider to identify underlying causes, such as structural abnormalities or immune system issues. Exploring long-term preventive strategies, such as low-dose antibiotics or specialized therapies, can be crucial in minimizing the recurrence of infections.