A Detailed Journey Through Laparoscopic Inguinal Hernia Surgery.
Laparoscopic inguinal hernia surgery, a modern and minimally invasive approach to hernia repair, has gained prominence for its efficacy and quicker recovery times compared to traditional open surgeries. In this comprehensive guide, we will delve into the intricate steps involved in laparoscopic inguinal hernia surgery, shedding light on the procedure’s nuances and benefits.
Introduction to Laparoscopic Inguinal Hernia Surgery: Laparoscopic inguinal hernia surgery is a technique that utilizes small incisions and a camera-equipped laparoscope to repair hernias in the inguinal region, which is the groin. Unlike traditional open surgeries, this minimally invasive approach offers reduced postoperative pain, shorter hospital stays, and a quicker return to normal activities.
Patient Preparation: Before the surgery begins, the patient undergoes a thorough preoperative evaluation. This includes a physical examination, medical history review, and possibly imaging studies to precisely identify the location and size of the hernia. Patients are typically instructed to refrain from eating or drinking for a specified period before the surgery.
Anesthesia Administration: Once the patient is prepared, anesthesia is administered. In laparoscopic hernia surgery, this is often done using general anesthesia to ensure the patient remains unconscious and pain-free throughout the price
Creation of Incisions: The surgeon makes small incisions in the abdominal wall, through which trocars (narrow tubes) are inserted. These trocars serve as entry points for the laparoscope and specialized surgical instruments.
Insufflation of the Abdomen: To create a working space, carbon dioxide gas is gently introduced into the abdominal cavity. This process, known as insufflation, lifts the abdominal wall away from the internal organs, providing the surgeon with a clear view and ample space to work.
Introduction of the Laparoscope: A laparoscope, a thin tube with a light and camera on the end, is inserted through one of the trocars. This enables the surgical team to visualize the hernia and surrounding structures on a monitor in real-time.
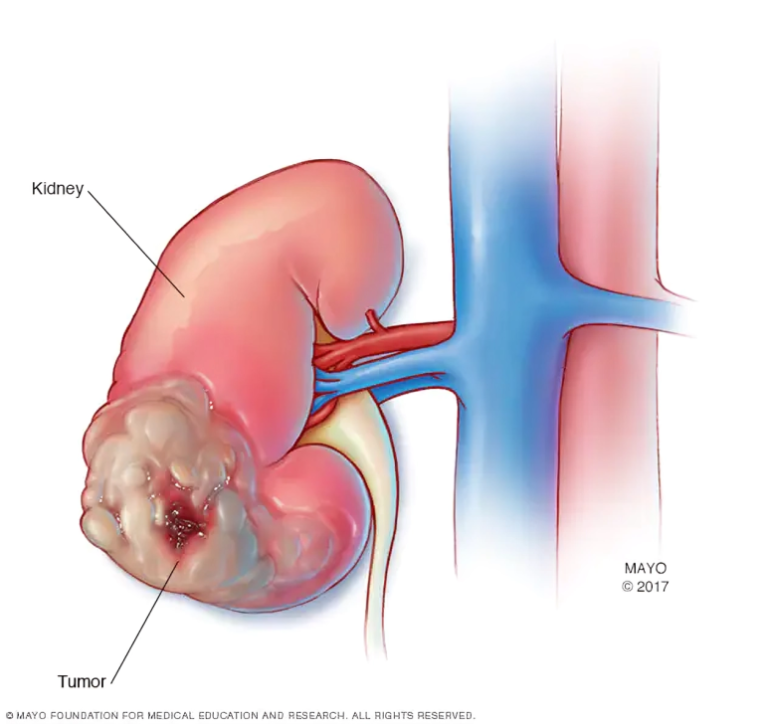
Identification and Reduction of the Hernia: The surgeon carefully identifies the herniated tissue and gently pushes it back into its normal position. This process, known as reduction, is a crucial step in hernia repair.
Mesh Placement: A synthetic mesh is then placed over the hernia defect to reinforce the weakened area and prevent a recurrence. The mesh is secured in place using specialized instruments and techniques.
Closure of Incisions: With the hernia repaired, the surgeon removes the laparoscope and any remaining instruments. The small incisions are then closed with stitches or surgical tape. Compared to traditional open surgery, the incisions in laparoscopic hernia repair are significantly smaller, leading to less scarring.
Recovery and Postoperative Care: Following laparoscopic inguinal hernia surgery, patients generally experience less pain and a faster recovery. Most individuals can resume light activities within a week, with a gradual return to normal routines over the following weeks. Postoperative care involves pain management, monitoring for any signs of infection or complications, and a follow-up schedule with the surgical team.
Conclusion: Laparoscopic inguinal hernia surgery stands as a testament to the advancements in modern surgical techniques. Its step-by-step approach, from patient preparation to postoperative care, emphasizes the precision and efficiency of this minimally invasive procedure. As technology continues to evolve, laparoscopic techniques are likely to become even more refined, offering further benefits to patients seeking effective hernia repair with minimized impact on their daily lives.